Abstract
This descriptive research study aimed to examine the perceptions non-circumcising American families had of healthcare providers (HCP) knowledge and attitudes and to explore how these perceptions impact their decision-making. This inquiry utilized a Community-Based Participatory Research (CBPR) model and Leiningers Theory of Culture Care Diversity and Universality as the framework. Conversations with the partnered community indicate intact is the preferred terminology of a noncircumcising child. A 16-item primary investigator tool was used to assess perceptions of respondents experiences with healthcare. The analysis revealed several significant findings and was themed accordingly. Knowledge responses revealed that parents had concerns regarding HCP understanding of appropriate intact care practices. More than 60% of parents not holding a healthcare degree (HCD) agreed that knowledge concerns impacted their healthcare decisions and approximately 23% missed a well-child appointment due to concerns over HCP knowledge of intact care. Attitude responses found that parents generally agreed with feeling supported and respected by their HCP. However, 63% of non- HCD parents results revealed concerns about HCPs attitude that impacted healthcare decision making. Experiential perceptions results indicated that 31% of the non-HCD parents agreed that their childs foreskin had been inappropriately retracted, 74% agreed it was difficult to find an HCP who is knowledgeable regarding intact care, and 66% agreed with being worried about seeking care because of concerns related to an HCP causing harm. These results speak to the importance of accurate provider knowledge and understanding of intact care and providing appropriate information and advice.
Keywords: intact care, non-circumcising, forced retraction, community based participatory research (CBPR), quality and safety education for nurses (QSEN), cultural competence
Introduction
Current trends in the United States indicate routine infant circumcision (RIC) has declined for the past thirty years, with recent data estimating a newborn circumcision rate of less than 60% on a national level (Center for Disease Control and Prevention, 2011; Owings, Uddin & Williams, 2013). Since these figures were reported, the American Academy of Pediatrics (AAP, 2012) issued a revision of its position statement on RIC, indicating that while the AAP found benefits to the procedure, these were insufficient to routinely recommend circumcision for all male infants. With more parents electing to forgo the procedure for their sons, it is anticipated that nurses and other healthcare providers (HCP) will care for an increasing number of intact (non-circumcised) male patients in the coming years.
Nursing, as a professional discipline, embraces efforts to provide care that is respectful, integrative and family-centric. This model benefits the patients and families (Coyne, 2015). In examining methods to further these efforts, the family experience must be considered, including the family perceptions of attitudes held by HCPs
Attitude has been characterized in the literature as having three major defining components: (a) a mental state-conscious or unconscious; (b) a value, belief, or feeling; and (c) a predisposition to behavior or action (Altmann, 2008).
Background
Despite an exhaustive review of the research, not a solitary empirical article in nursing, or any other allied health discipline, could be located exploring the perceptions of non-circumcising American families in the health system. In an attempt to locate any work of relevance to the research aims, a wide variety of individual and combinations of search terms were utilized, including intact care, uncircumcised boys care, un-circumcised boys care, non-circumcising families, uncircumcised boys, intact care nursing, penis care, parent perceptions and many more. Multiple databases and search engines were employed, including CINAHL, PubMed and Google Scholar for articles related to intact care published in English between 2009 and December 2018.
While care recommendations and web-based guides were located, no relevant empirical articles could be found. Among the care guides located, there was considerable variation in the recommendations offered, and none were offered as a formal guideline to be used in the education of nurses or other health professionals. The search did yield an abundance of reviews of the available literature surrounding the practice, ethics, and legality of the circumcision procedure itself, but these were omitted as they did not fall within the scope of this research. Rather, the purpose of this work was to explore this changing cultural practice from the perspective of non-circumcising American families as consumers of health care and to learn about their perceptions of HCP knowledge and attitude regarding the care of their intact children. An additional goal was to gather information on how these perceptions impact the healthcare decision-making of these families. With nurses often being among the first HCP to interact with and educate new families, this work was appropriately aligned with nursings scope and desire for patient advocacy and culturally competent care.
Significance
Methods
Theoretical Framework
Leiningers Theory of Culture Care Diversity and Universality was utilized as a theoretical framework for this study and applied to a model of Community-Based Participatory Research (CBPR) in the virtual setting. This theory offered applicability to the goal of helping professional nurses with understanding differences in caring for individuals and families of various cultural backgrounds. Leiningers (n.d.) definition of culture is not limited by ethnicity and allows for groupings of individual of shared beliefs and values. Culture is defined as the learned, shared and transmitted values, beliefs, norms, and lifeways of a particular culture that guide thinking, decisions, and actions in patterned ways and often inter-generationally (Leininger & McFarland, 2002, p. 47). Given the expansive social networks within the virtual setting, individuals are now capable to connect with communities of shared beliefs without being restricted by ethnicity and geography. This definition also plays well with the concepts included in the CBPR model, which is defined as a collaborative research approach that is designed to ensure and establish structures for participation by communities affected by the issue being studied, representatives of organizations, and researchers in all aspects of the research process to improve health and well-being through taking action, including social change (AHRQ, 2004, para 1).
Research Question
The purpose of this work was to explore the perceptions of non-circumcising American families of HCP knowledge and attitude regarding intact care and how these perceptions influence their healthcare decision-making. Gaining this insight could assist nurses and other HCPs in enhancing the delivery of culturally competent, family-centered care for intact patients and their families.
Design
To access the population of interest, the CBPR model was employed in a virtual community using social media. Multiple groups exist for parents of intact children on this platform, but many are hidden from Public view and remain Secret. The research team was able to access the population of interest through a partnership with one such community, being allowed entry into the virtual group. After months of listening, relationship-building and establishing trust, through nonjudgmental community interaction, the researchers found the virtual community to become enthusiastic, supportive and excited about being a part of the nursing research, and eager to have a venue through which to share their experiences and perceptions with the health system.
There are numerous advantages to utilizing this model. One benefit of the virtual community is the ability to engage a number of individuals of similar health beliefs who may be geographically beyond the capacity of the research team in any other setting. In numerous instances, specific societies and clusters of groups prevail exclusively in the virtual world (Belone et al, 2016). Although individuals surely debate such concerns with family, friends, and colleagues, only a few connect in person to talk about the issues (Belone et al, 2016). Anecdotally, many participants reached out to the research team using the contact information located in the consent document to share their poor experiences with the health system; a sharing of information that likely would have been limited without the anonymity offered by virtual interaction.
This descriptive research survey study was conducted through a partnership with the leader and moderator of a large private social media group for parents of intact children. The survey utilized was a 16 item, primary investigator-developed instrument that included demographic questions and six-point Likert-style items rating agreement or disagreement with statements regarding parental perceptions. A principle investigator tool was utilized as no existing instrument was able to be located that had been validated in measuring the parental perceptions. An informed consent item was embedded at the beginning of the survey.
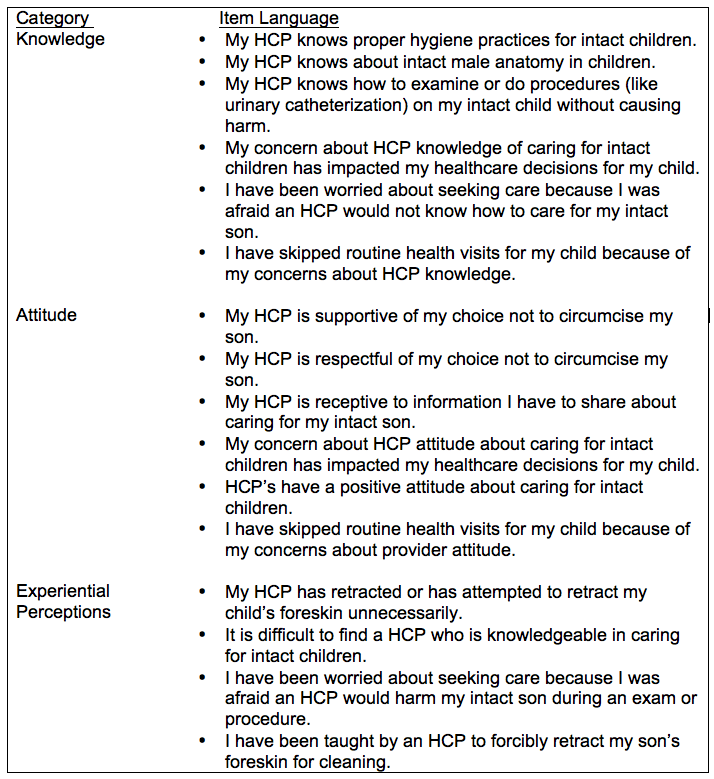
The development of the instrument was informed by consideration of the Quality and Safety Education for Nurses (QSEN) competencies (2018) including evidence-based practice (EBP), patient-centered care and safety, and the CBPR model. The overall goal of QSEN (2018) is to meet the challenge of future nurses who will have the knowledge, skills, and attitudes necessary to continuously improve the quality and safety of the healthcare systems within which they work (para.1). With this being a major force in quality improvement initiatives in the nursing profession, the decision was made to align the study concepts with the QSEN project concepts. This was solely done with the intention of making any identified concerning parental perceptions most amenable to intervention. Items have been categorized in Table 1 below.
Table 1. Survey Items Categorized for Analysis
Statistical Analysis
Sample
A total of 530 unique respondents completed the survey and met all inclusion criteria, being an American parent of an intact son between birth and 10 years of age who acted as a primary decision-maker for health care. The majority of the respondents (87%) were between 26 to 44 years of age and 80% indicated Caucasian as their ethnicity. Interestingly, a large percent (23%) of the survey respondents identified as having a healthcare degree (HCD), with an additional 45% of respondents having at least a college degree or higher. The remaining respondents had some or no college education. All respondents were recruited through convenience sampling. The survey was introduced as a link in a social media post by both the authors and the moderator of the virtual partner community. Survey spread was impossible to track as participants shared the link widely. The survey was closed for analysis after 36 hours of being live, after far exceeding recruitment goals. As no identifying data was collected and no interaction took place between the authors and the respondents, this study was reviewed and determined to have exempt status designation through the Oakland University Institutional Review Board.
As this data was descriptive in nature and there was no comparison group, relationships were identified during the analysis. Patterns were noted between respondents who self-identified as having an HCD (n=125) and those who held all other levels of education (n=405). Results were organized according to knowledge, attitude, and other experiential healthcare perceptions. General questions asked included what the participants primary source of health care was and what was the primary source of information for education regarding genital hygiene.
Data analysis was conducted utilizing SPSS version 18. Analysis was performed through frequencies, distributions and Pearsons correlations.
Results
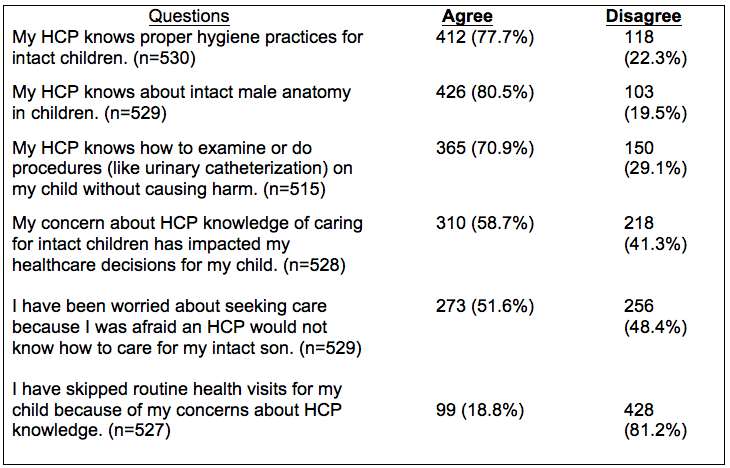
Data was organized into categories of knowledge, attitude and experiential item responses. Responses were organized into any degree of agreement or disagreement, as no neutral option was presented. Results were initially analyzed from the total population, then isolated by level of education for comparison. In examining the total population (see Table 2), results revealed concerns regarding HCP knowledge of intact care. Of the total sample, 22.3% disagreed that their HCP was knowledgeable about proper hygiene, 19.5% disagreed that their HCP was knowledgeable about intact male anatomy, 29.1% disagreed that their HCP knew how to do exams or procedures on an intact child. Regarding parental healthcare decision making, 58.7% agreed that their concern about HCP knowledge had impacted their decision making, 51.6% were worried about seeking care due to limited provider knowledge, and 18.8% agreed that they intentionally missed a well visit due to concerns about adequate HCP knowledge.
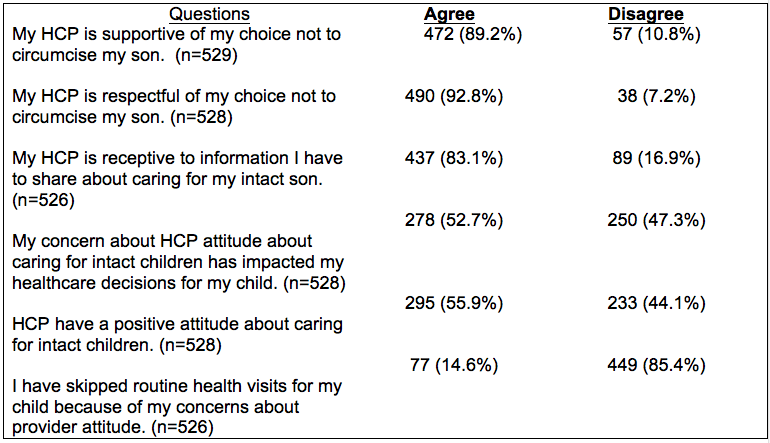
When responding to attitude (see Table 3) items regarding parental perceptions of their HCP, 89.2% agreed with feeling supported in the choice to leave their son intact, 92.8% agreed their HCP was respectful of the decision to leave their son intact, and 83.1% agreed their provider was receptive to information shared regarding care and hygiene. In response to items regarding HCPs in general, perceptions of attitude were less favorable with 55.9% agreeing that HCPs have a positive attitude about caring for intact children, 52.7% agreeing that provider attitude has impacted their health care decision-making, and 14.6% had acknowledged missing a well-visit due to concerns regarding provider attitude.
Table 2. Results from total sample Knowledge Survey Items Categorized for Analysis
Table 3. Attitude Survey Items Categorized for Analysis (Results from total sample)
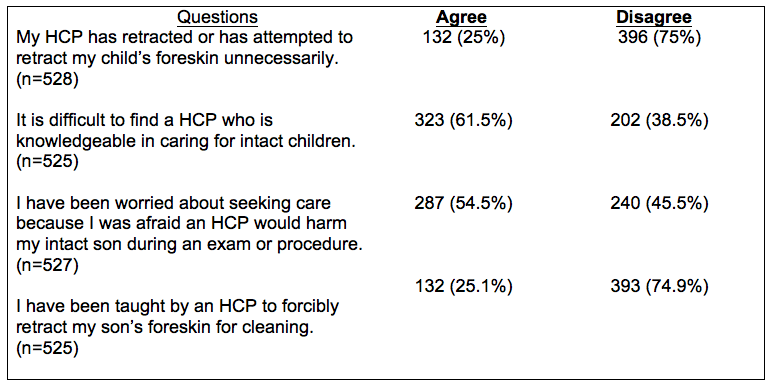
In regards to parents healthcare experiences (see Table 4), 25% reported an HCP had retracted or attempted to retract their childs foreskin unnecessarily and 25.1 % agreed with reported being taught by an HCP to retract their childs foreskin for hygiene. Additionally, 61.5% agreed it was difficult to find an HCP knowledgeable of intact care and 54.5% agreed they worried about seeking care due to fear an HCP would harm their child during exams or procedures. Patterns of responses noted during general analysis led to further examination of categorical findings and isolation of groups for comparisons.
Outcomes
Knowledge – As data were examined, patterns of responses became evident, and participant groups were isolated for comparison. Differences existed in the perceptions of provider knowledge between parents who self-identified as having an HCD and parents who identified with any other level of education. HCD parents consistently responded more positively in regards to perceptions of HCP knowledge.
Responses to the knowledge items revealed parent concerns for provider knowledge of intact care. These concerns included 68.8% (n=279) of non-HCD parents agreeing that these concerns have impacted healthcare decisions and approximately 23.2% (n=94) agreeing that these non-HCD parents had avoided a well-child appointment for this reason. Higher levels of education were inversely correlated to agreement with these items. Implications of these findings are explored in the discussion, below.
Attitude – Comparison groups were identified in the same manner as the knowledge items. Differences between parents with HCDs and those with all other levels of education continued to be apparent. While parents generally agreed with feeling supported and respected, HCD-holding parents agreed more frequently than non-HCD parents. In this group, (non-HCD parents) and having concerns about attitude impacted healthcare decision-making for 62.9% (n=255) of respondents and 18% (n=73) correlated with having missed a well-visit due to concerns over provider attitude about caring for intact children. This avoidance also was found to be statistically inversely correlated with level of education.
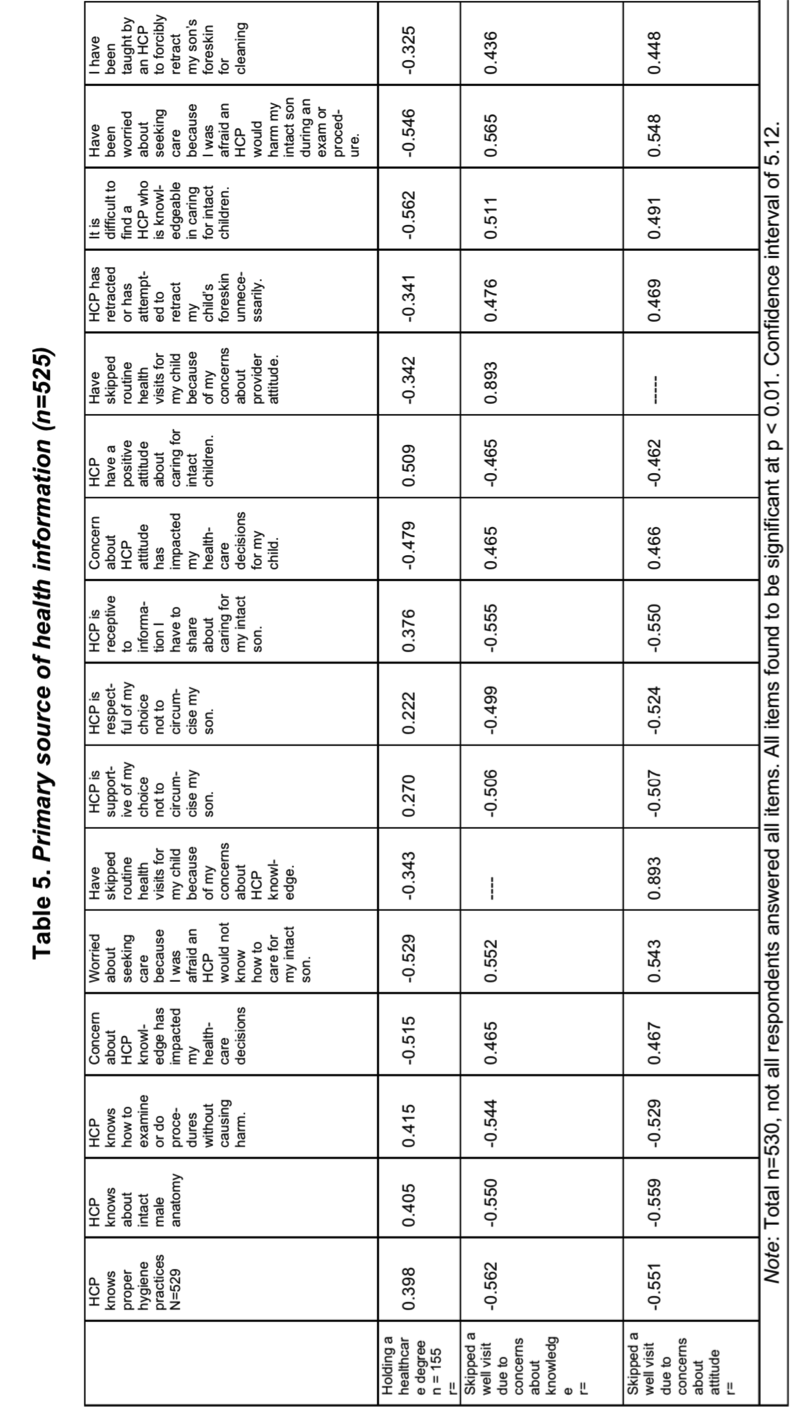
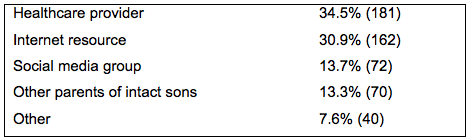
Experiential Perception – Differences emerged between HCD-holding and non-HCD-holding parents in experiential perceptions as well (see Table 4). Of the non-HCD group, 30.6% (n=124) agreed that their childs foreskin had been inappropriately retracted, 73.3% (n=297) agreed it was difficult to find an HCP who is knowledgeable regarding intact care, 65.9% (n=267) agreed with being worried about seeking care because of concerns a provider would harm the intact child and 29.8% (n=121) had been taught to retract the childs foreskin for cleaning. Parents holding an HCD had much less frequent agreement on all items and having a healthcare degree was found to be inversely correlated statistically with these experiences (see Table 5). To provide context to the survey responses, respondents were also asked what their primary source of health information was (see Table 6).
Table 4. Results from total sample experiential perceptions survey items categorized for analysis
Table 5.
Table 6. Primary source of health information (n=525)
Discussion
Examining the findings in the context of the health system offers multiple points for discussion. In keeping with the structure used to provide a framework to the survey, these points are organized as pertinent to knowledge, attitudes, and experience.
Knowledge – Parents perceived provider knowledge of intact care less favorably than anticipated. Because the survey did not assess which HCP the parent was observing or the context of the interaction, interpretations cannot be made of provider knowledge. However, these findings suggest further investigation of actual HCP knowledge may provide additional insight. Provider knowledge is vital not only for the facilitation of trust between the HCP and the parent but for the rendering of safe care (Mollon, 2014). If provider knowledge is truly as low as it is perceived by parents, there is significant potential for harm to the intact child during examinations or procedures. This low perception of knowledge may partially explain the low portion of the survey population that identified their HCP as a primary source of information regarding genital hygiene.
With RIC rates declining, and additional national attention being given to this issue, providers are obligated to ensure accurate knowledge and practices for the care of these children (Warner et al. 2015). Recently, a lawsuit was filed against a registered nurse (RN) in Georgia for alleged forcible retraction of the foreskin of an intact infant male, despite his mothers objections (Fulton County State and Magistrate Court, 2018). This case presents an example of the liabilities associated with improper intact care.
Additionally, the identification of parents perceptions of low HCP knowledge as a factor in missed well-child visits is concerning. Of those parents without an HCD, 23% agreed that apprehensions over provider knowledge of intact care had caused these parents to miss a routine health maintenance appointment. In early childhood, the impact of these missed visits can be significant. Weight monitoring, growth and developmental surveillance, vaccinations and health screenings occur in these visits and promote optimal health outcomes (Abdus & Selden, 2013), making this finding of particular interest to advanced practice nurses in the primary care setting. Lack of follow-up is even more concerning in children with chronic health needs, as they require more frequent care and monitoring (Schuster, Chung & Vestal, 2011). Providers must minimize barriers to well-child care, foster trust, and practice in a way that is consistent with guidelines and current evidence so as to promote the best patient engagement in their health care.
Attitude – The overwhelming majority of parents agreed with feeling supported and respected by HCPs, which is a powerful testament to the increased focus in todays health system on family-centered care and cultural competence (Davies et al. 2017). Conversely, findings from this study indicate ramifications of parents not feeling supported or respected in health decisions for their children. Of the non-HCD parents, 18% agreed with having missed a well visit due to provider attitude. Despite much more positive findings in this category, this is still a significant percentage that could have serious implications for the children involved. The virtual community in which the survey was introduced keeps a community generated list of intact friendly providers to refer to. These providers have been identified by the community as being generally supportive in attitude and accurate in knowledge. This list has become the communitys own intervention to address the concerns over provider knowledge and attitude and minimize missed visits.
Experiential Perceptions – The most worrisome of the survey findings were possibly those classified as experiential. These questions were asked to give insight into the patients experiences and provide some context to their responses. Nearly 1 in 3 non-HCD-holding parents agreed that their intact sons had had their foreskins inappropriately retracted, an unnecessary and potentially traumatic practice (Abbas & McCarthy, 2016). Additionally, approximately 1 in 3 non-HCD-holding parents agreed with having been taught by an HCP to do this regularly to clean their intact child. This antiquated practice reflects a lack of knowledge of the physiologic development and function of the foreskin on the part of HCPs and presents a major challenge to the provision of safe patient care to intact children in the health system (Hunter, 2012).
Limitations
While this study provides valuable insight into perceptions of non-circumcising American families as consumers of health care, several limitations must be acknowledged. Most obviously, the lack of pertinent literature on the experience of these families gave little context for the work. The research team, beyond consultation with the partner community, was without resource in constructing the study survey or focusing the aims of the survey. Additionally, online data collection limitations include the population samples and the nonrandom nature. This survey was linked to a social media site and solicited volunteers to fill out the survey. Since the survey was delivered through social media, it is acknowledged that some potential respondents may lack the ability to use the new technology or the willingness to participate in online computer surveys.
One significant limitation was the lack of a standardized instrument available to measure participant perceptions. The researchers were therefore forced to create items that were commonly acceptable to accommodate the partner virtual community of parents of intact sons. While every effort, including the review of the instrument by experts in pediatrics and research, was made to ensure content and language were appropriate, neutral and inclusive through face validity, it was impossible to eliminate a possible influence of the wording used in this article. In attempting to manage this limitation, the partner community was engaged in language development for items for measurement. This process is considered one of the advantages of the CBPR model and can allow for the development of instruments that are as culturally acceptable to the partner community as possible (Belone et al. 2016; Schensul et al. 1987, as cited in AHRQ, 2004). Further limitations were presented by the homogeneity of the sample, making it difficult to generalize the findings outside of the Caucasian population. While this survey was initially introduced within a virtual community for parents of intact sons residing in a single American Midwest state, participants shared the survey posted to numerous other state and national groups. This is a constraint that must be addressed in the future to include questions regarding the residential state, whether this was their first born intact child, age and sex of primary caregiver, and finally the ethnicity of the provider.
Recommendations for Future Research
Future research will assess the realities of the HCP knowledge gap for the best facilitation of nursing quality improvement. Nurses can be instrumental in improving these negative perceptions through a commitment to cultural competence, EBP, and patient advocacy for the non-circumcising family accessing the healthcare system. Health systems engaged in quality improvement regarding intact care practices would be advised to consider publication of their effort to contribute to the body of knowledge surrounding the issue. Presently, there is a paucity of literature available on the topic. Additionally, clarification of care guidelines is necessary to accomplish this end.
Implications for Nursing Practice
Knowledge of the intact male anatomy and its appropriate care is an essential responsibility of nurses in all practice settings, regardless of the beliefs or preferences of the individual clinician. Patient safety and culturally competent care are dependent on bedside nurses and other HCPs being knowledgeable in the functions and development of the male foreskin and performing procedures and hygiene in ways that do not cause harm.
Nurses and other HCPs must understand that patient perception is their reality (Rannan-Eliya et al. 2015). When patients question the knowledge level of their providers or feel judged in their health decision-making, this can negatively impact their relationship with the health system and their outcomes (Wessel et al. 2013). Furthermore, with American parents becoming an increasingly health literate group of consumers, nurses practicing outside the realms of accurate intact care knowledge could potentiate legal compromise for themselves and their health systems. Diligent and up-to-date practice that is informed by an accurate understanding of the intact male body and the relevant evidence is needed to render safe and responsible care.
Conclusion
A fundamental goal of nursing is to provide care that is person-centered, caring and culturally appropriate. With American culture shifting position on routine infant circumcision, nurses are likely to encounter intact male patients and their families. For some of these patients, rejection of the circumcision procedure may represent a cultural or personal value that requires nursing sensitivity and cultural competence. Thus, Leiningers Theory of Transcultural Care can offer guidance in the provision of nursing care to these clients.
This descriptive research study explored the perceptions of non-circumcising families and the subsequent impact on healthcare decisions through partnership with a virtual community for parents of intact male children, utilizing this theory as a framework. The results indicated, even when parents perceived their HCPs to have positive attitudes regarding intact care, that parental perceptions of nurses knowledge were low. This had implications for healthcare decision-making. This speaks to the importance of accurate HCP knowledge and understanding of intact care so as to optimize the patient experience and health outcomes.
Acknowledgements
The research team wishes to thank Jennifer DJamoos, co-director of Intact Michigan, who welcomed this effort and inquiry and whose partnership was instrumental for its success, and Margaret Harris, Ph.D., RN, Zorica Kauric-Klein, PhD, APRN-BC, and Jeffrey Ormond for their thoughtful review of this work during its early stages. This work required no funding and therefore has no funding disclosures/acknowledgements. The authors declare no conflicts of interest.
References
Abbas, T., & McCarthy, L. (2016). Foreskin and penile problems in childhood. Surgery (Oxford), 34 (5), 221-225. doi:10.1016/j.mpsur.2016.03.007
Abdus, S., & Selden, T. M. (2013). Adherence with recommended well-child visits has grown, but large gaps persist among various socioeconomic groups. Health Affairs (Project Hope), 32 (3), 508.
Agency for Healthcare Research and Quality, (2004). Community-based participatory research. Publication Number 04-E022-1, Retrieved from https://archive.ahrq.gov/clinic/epcsums/cbprsum.htm
Altmann, T. (2008). Attitude: A concept analysis. Nursing Forum, 43 (3), 144-150, doi: 10.1111/j.1744-6198.2008.00106.x.American Academy of Pediatrics, (2017). Care for an uncircumcised penis. Retrieved from https://www.healthychildren.org/English/ages-stages/baby/bathing-skin-care/Pages/Care-for-an-Uncircu….
American Academy of Pediatrics Task Force on Circumcision. (2012). Circumcision policy statement. Pediatrics, 130 (3), 585.
Belone, L., Lucero, J., Duran, B., Tafoya, G., Baker, E., Chan, D., . . . Wallerstein, N. (2016). Community-based participatory research conceptual model: Community partner consultation and face validity. Qualitative Health Research, 26(1), 117doi.org/10.1177/1049732314557084
Cacari-Stone, L., Wallerstein, N., Garcia, A. P., & Minkler, M. (2014). The promise of community-based participatory research for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health , 104 (9), 16151623. http://doi.org/10.2105/AJPH.2014.301961
Centers for Disease Control and Prevention, (2011). Trends in in-hospital newborn male
circumcision — United States, 1999–2010. Morbidity and Mortality Weekly Report (MMWR) 60(34);1167-1168. CO: Westview Press, 1987.
Coyne, I. (2015). Families and health-care professionals’ perspectives and expectations of family-centered care: hidden expectations and unclear roles. Health Expect, 18: 796808. doi:10.1111/hex.12104
Davies, B., Steele, R., Krueger, G., Albersheim, S., Baird, J., Bifirie, M., . . . Zhao, Y. (2017). Best practice in Provider/Parent interaction. Qualitative Health Research, 27 (3), 406-420. doi:10.1177/1049732316664712
Douglas, M.K. et al., (2014). Guidelines for implementing culturally competent nursing care. Journal of Transcultural Nursing , 25(2),109 121. doi:org/10.1177/1043659614520998
Fulton County State and Magistrate Court (2018). Case information: 18EV000194. Retrieved from https://publicrecordsaccess.fultoncountyga.gov/Portal/Home/WorkspaceMode?p=0
Hunter, D. (2012). Conditions affecting the foreskin. Nursing Standard (through 2013), 26 (37), 35-9. doi:10.7748/ns2012.05.26.37.35.c9109
Leininger, M. (2002). Culture Care Theory: A Major Contribution to Advance Transcultural Nursing Knowledge and Practices. Journal of Transcultural Nursing, 13 (3), 189-192.
Leininger, M., & McFarland, M. (n.d.). Transcultural nursing: Concepts, theories, research, and practice (3rd ed.). New York: McGraw-Hill, Medical Pub. Division: 2002.
Mollon, D. (2014). Feeling safe during an inpatient hospitalization: A concept analysis. Journal of Advanced Nursing, 70 (8), 1727-1737. doi:10.1111/jan.12348
Munyan, K. & Wodwaski, N. (2019). A survey of American nurses: Attitudes regarding circumcision and care of the intact male patient. International Journal of Healing and Caring, 1 (1).
Owings, M., Uddin, S., & Williams, S., (2013). Trends in Circumcision for Male Newborns in U.S. Hospitals: 1979-2010. Retrieved from www.cdc.gov/nchs/data/hestat/circumcision_2013/circumcision_2013.pdf
QSEN (2018). QSEN Competencies. Retrieved from http://qsen.org/competencies/pre-licensure-ksas/
Rannan-Eliya, R. P., Wijemanne, N., Liyanage, I. K., Jayanthan, J., Dalpatadu, S., Amarasinghe, S., & Anuranga, C. (2015). The quality of outpatient primary care in public and private sectors in Sri Lanka–how well do patient perceptions match reality and what are the implications? Health Policy and Planning, 30 Supplement 1 (suppl 1), i59-i74. doi:10.1093/heapol/czu115
Schensul, J., Denelli-Hess, D., Borreo M., et al. (1987). Urban comadronas: Maternal and child health research and policy formulation in a Puerto Rican community. In: Stull DD, Schensul JJ, eds. Collaborative Research and Social Changes: Applied Anthropology in Action . Boulder, CO: Westview Press.
Schuster, M. A., Chung, P. J., & Vestal, K. D. (2011). Children with health issues. The Future of Children, 21 (2), 91-116. doi:0.1353/foc.2011.0017
Warner, L., Cox, S., Whiteman, M., Jamieson, D. J., Macaluso, M., Bansil, P., . . . Barfield, W. D. (2015). Impact of health insurance type on trends in newborn circumcision, United States, 2000 to 2010. American Journal of Public Health, 105 (9), 1943-1949. doi:10.2105/AJPH.2015.302629
Wessel, M., Helgesson, G., Olsson, D., Juth, N., Alexanderson, K., & Lyne, N. (2013). When do patients feel wronged? Empirical study of sick-listed patients’ experiences with healthcare encounters. European Journal of Public Health, 23 (2), 230-235. doi:10.1093/eurpub/cks030
Kristen Munyan, DNP, RN, MSN-Ed, FNP-BC is an Assistant Professor in the School of Nursing at Oakland University. She obtained a Masters of Nursing Education from Oakland University and her Doctor of Nursing Practice and nurse practitioner training at Wayne State University where her work focused on preparing home health nurses to respond to tracheostomy emergencies in the ventilator-dependent homebound pediatric population through the use of simulation learning methodology. Now practicing as a Family Nurse Practitioner, Dr. Munyan’s research focuses on the translation of evidence to clinical care and health care access in rural settings. Topics of interest to Dr. Munyan include intact care, the usefulness of leveraging social media in reaching marginalized patient populations and the utilization of telehealth to remove barriers to care.
Contact:
Oakland University
318 Meadow Brook Rd
Rochester, MI. 48309
kmunyan@oakland.edu
Nadine Wodwaski, DNP, MSN-ed, RN, ACNS is an Assistant Professor at the University of Detroit Mercy McAuley School of Nursing. She has had the pleasure of caring for clients in the community and acute care setting. She has practiced in emergency, maternal child, med/surg, and the cardiac catheterization lab. As an advanced practice nurse, she strives to improve healthcare through evidence-based practice at the individual patient and systems levels. As an academician, she has elected to focus on caring behaviors, intact care, and emotional intelligence in her research. Promoting expressive caring is a worthy and even an important aim, achievable by focusing on evidence that is based on compassionate caring.
Contact:
University of Detroit Mercy
4001 W. McNichols Rd
Detroit, MI. 48221
wodwasnk@udmercy.edu
(248) 719-1865